First of all,
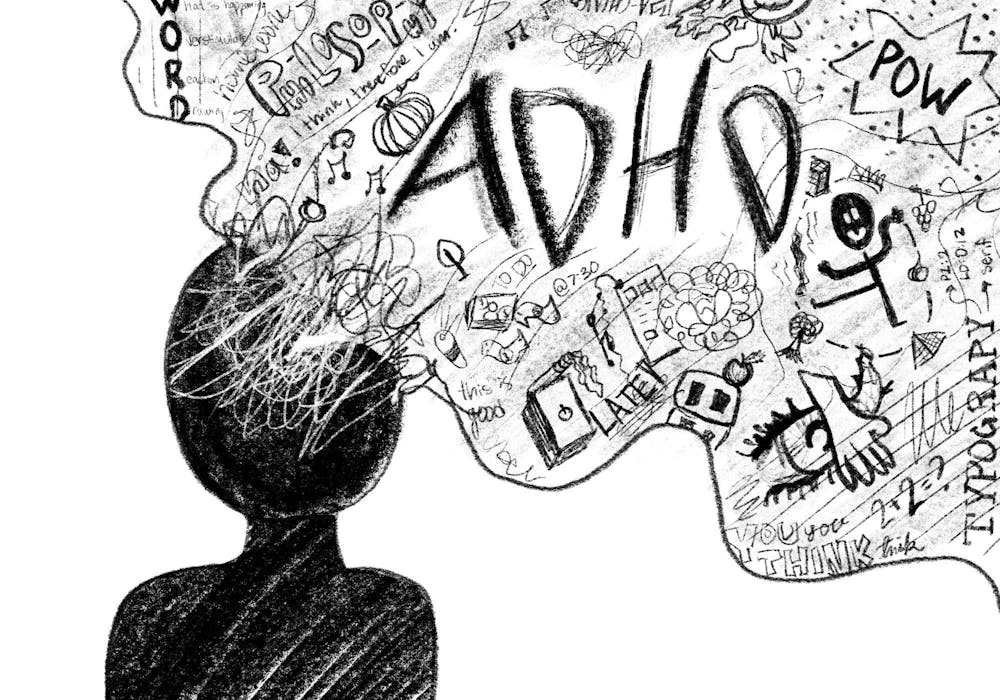
The neurodevelopmental disorder known as Attention Deficit Hyperactivity Disorder (ADHD) is typified by impulsivity, hyperactivity, and inattention. Although it affects people of all ages, childhood diagnoses are the most common. Traditionally, stimulant drugs such as amphetamine (Adderall) and methylphenidate (Ritalin) have been the mainstay of ADHD treatment. But there has been a recent upsurge in interest in and research into creating novel drugs with different modes of action and maybe fewer adverse effects. This article explores the novel approaches, difficulties, and therapeutic prospects for ADHD medicines, delving into the recent developments in this field.
Comprehending the Conventional Method of ADHD Medication Administration:
Because stimulant drugs increase brain levels of dopamine and norepinephrine, which improve attention and impulsive control, they have long been the mainstay of treatment for attention deficit hyperactivity disorder (ADHD).
ADHD symptoms have been effectively managed by methylphenidate and amphetamine-based medications; however, these drugs come with possible adverse effects, including decreased appetite, sleeplessness, and potential for misuse.
Those who are unable to take stimulants or have a history of substance misuse may find alternatives in non-stimulant pharmaceuticals such as guanfacine (Intuniv) and atomoxetine (Strattera). They might not be as effective as stimulants, though.
The Development of New ADHD Drugs:
The development of innovative ADHD drugs with distinct modes of action or that target alternative neurotransmitter systems has garnered increased attention in recent years.
Noradrenergic alpha-2 agonists, which include clonidine and guanfacine extended-release, are one potential family of drugs. Without having the stimulant effects of conventional ADHD treatments, these therapies improve attention and impulse control by modifying norepinephrine levels in the prefrontal cortex.
Glutamatergic drugs,
Which target the glutamate neurotransmitter pathway linked to ADHD, are another rapidly developing field of study. In tiny trials, drugs like memantine and ketamine have demonstrated some efficacy, but further research is required to determine their safety and efficacy.
Furthermore, there is increasing interest in using already-approved drugs to treat ADHD. Modafinil, for instance, a wakefulness-promoting medication used to treat sleep disorders, has demonstrated potential in reducing symptoms of ADHD in certain people.
Obstacles in the Development and Use of Novel ADHD Drugs:
Novel ADHD drugs have great potential, but their research and application are fraught with difficulties.
Recruiting participants for clinical studies involving ADHD drugs can be difficult because of the disorder’s heterogeneity and individual differences in treatment response.
When developing new drugs, safety considerations—such as the possibility of addiction or long-term negative effects—are crucial, especially for young patients.
The cost and insurance coverage of novel ADHD drugs may restrict access, making therapy unattainable for those from lower socioeconomic backgrounds.
The Prospects for ADHD Drug Development:
Personalized therapy techniques that consider individual differences in symptom presentation, hereditary variables, and treatment response hold the key to the future of ADHD medicine.
Pharmacogenetics advances may make it possible to find genetic markers that indicate how a patient will react to a particular drug,
Enabling more focused treatment approaches.
When compared to single-agent treatments, combination therapies that target multiple neurotransmitter systems at once may be more effective and tolerable.
With its ability to provide behavioral interventions and real-time symptom monitoring, digital therapeutics—such as wearable technology and smartphone apps—have great potential as supplementary therapies for ADHD.
Innovation in ADHD medicine
Will be fueled by ongoing research into the neurology of the disorder and the discovery of new therapeutic targets, which will ultimately improve results for those who suffer from the condition.
In summary:
The field of ADHD medication is changing quickly as researchers look into new therapeutic targets and creative ways to treat patients that go beyond stimulant-based treatments. Even if there are still obstacles in the way of developing and implementing new drugs, developments in personalized medicine, combination therapy, and digital medicines provide people with ADHD hope for better results. More research and a deeper knowledge of the neurobiology of ADHD mean that safer and more effective medicines that meet the many needs of people with this complex condition are likely to be developed in the future.